Every death by suicide is a shocking event, with wide-reaching consequences for loved ones, communities, and front-line professionals. Suicide prevention is a recognised health priority in England, and in early 2018, the Department for Health and Social Care, Public health England (PHE), and NHS England announced a three-year investment worth £25 million to support a country-wide reduction in suicide rates by 2021. Here, on World Suicide Prevention Day, Dr Pauline Turnbull explains how world-leading research at the University of Manchester will inform local quality improvement plans, to save lives and reduce suicide rates, both locally and nationally.
- The NCISH is a national project looking to improve safety for all mental health service users and reduce suicide rates
- Research has shown that implementation of NCISH’s recommendations by a particular health service has led to a reduction in suicides in that service
- A self-audit toolkit of 10 clinical standards which are associated with suicide reduction has been developed and work to deliver improvement locally in areas of England is underway
The National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH), which I project manage, collects detailed information on all suicides occurring in the UK, and has been running since 1996. Our overall aim is to improve safety for all users of mental health services. We provide crucial evidence to support service improvements and, ultimately, to contribute to a reduction in patient suicide rates and an overall decrease in the national suicide rate. We undertake studies into suicide prevention in the general population, and our core database is a UK-wide series of case studies that:
- Examines the circumstances leading up to and surrounding the deaths by suicide of people under the recent care of specialist mental health services;
- Identifies factors in the management and care of patients which may be related to suicide;
- Recommends measures to reduce the number of suicides by people receiving specialist mental health care
Recommendations and the economic cost of suicide
Our research has shown that implementing NCISH recommendations in health services is associated with a reduction in suicide rates within that service. There has been a decrease in suicides in specific high-risk settings that our recommendations targeted, including in-patients, crisis teams, and the post-discharge period. This work has contributed to an overall decrease in suicide nationally (estimated 250-300 fewer deaths per year). The economic cost of each suicide death is estimated to be around £1.67 million. Based on these figures, 300 fewer suicide deaths in England and Wales represent a potential cost saving of £500 million annually.
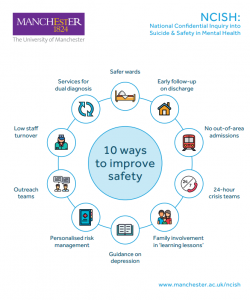
We formulated 20 years of NCISH recommendations into a self-audit toolkit of 10 clinical standards which are associated with suicide reduction – our “10 ways to improve safety”. These elements of safer care are presented as quality and safety statements about clinical and organisational aspects of care. They are intended to be used as the basis for self-assessment by specialist mental health care providers, and responses should ideally be based on recent local audit data or equivalent evidence.
Caption: NCISH’s 10 key elements for safer care of patients (Icons from Freepik)
Supporting quality improvement in local areas
As part of the £25 million government investment to reduce suicide rates, NCISH is now working with experts in Quality Improvement from the National Collaboration Centre for Mental Health (NCCMH) to support local areas to strengthen their suicide prevention plans. In particular, we are focusing on three of the main priority areas identified in the National Suicide Prevention Strategy:
- Mental health services;
- Self-harm services;
- Suicide prevention in men.
Funding has been allocated to eight NHS and local council sustainability and transformation partnerships (STPs) with a high level of need in the first year and learning from this first year of work will then inform suicide prevention quality improvement plans in the remaining STP areas nationally in years two and three. We are working with the Quality Improvement (QI) teams in each STP to provide expert knowledge of suicide prevention in the three priority areas, and to advice on local data collection. We are providing each area with bespoke data from our NCISH database, benchmarked against the national average, to help them review their services against established guidelines and recommendations, and to improve the quality of care they offer. Our previous work has shown us that adopting the recommendations from our “10 ways to improve safety” can reduce suicide rates. We would expect some of these safety elements to already be in place and are working with the STPs to identify which of the “10 ways” could be improved and embedded into local quality improvement plans.
Suicide prevention evidence in practice
We have long been aware of the impact of an NCISH recommendation in policy; we reported, for example, a 60% fall in deaths by hanging, on in-patient wards, following our recommendation to remove all non-collapsible curtain rails being adopted as an NHS ‘never event’.
Our current model of working directly with local areas marks an exciting new stage in our mission to improve safety for all mental health patients, and an opportunity to have an impact on suicide prevention in the general population.
We are keen to continue to explore ways to bring our research evidence into practice, and we are confident that this work with local quality improvement teams will help to improve standards of care, and ultimately, to save lives.